Flashes, Floaters, and an Unexpected POCUS Finding
This article also appears in the Southern Medical Association News at this link.
Case Presentation:
A 56-year-old male presented to his primary care provider with an acute onset of floaters and flashes of light in his left eye over the past two days. He denied trauma, headache, or systemic symptoms. His past medical history included hypertension and mild cataracts. On exam, his visual acuity was preserved at 20/25 in both eyes. Pupils were equal and reactive, and no afferent pupillary defect was noted. Fundoscopic examination was limited due to poor visualization of the posterior retina. Concerned about possible retinal pathology, the provider performed ocular point-of-care ultrasound (POCUS).
What do you see, and what’s the diagnosis?:
Clip 1. Ultrasound of the left eye demonstrating a hyperechoic membrane in the posterior chamber, tethered at the optic disc and lifted off the posterior wall on the right.
POCUS Findings:
The clip demonstrates a thin, hyperechoic, undulating membrane in the posterior chamber that is tethered at the optic disc and lifted off the posterior wall of the globe. This appearance is consistent with a retinal detachment. In this case, the detachment is localized to one side of the retina and does not include the macula, explaining why the patient’s vision remains relatively intact. In more advanced or complete retinal detachments, the retina appears as a thicker, flailing “ribbon” moving freely within the vitreous chamber, and is still tethered at the optic disc. Even small or partial detachments can progress and threaten central vision if not treated promptly.
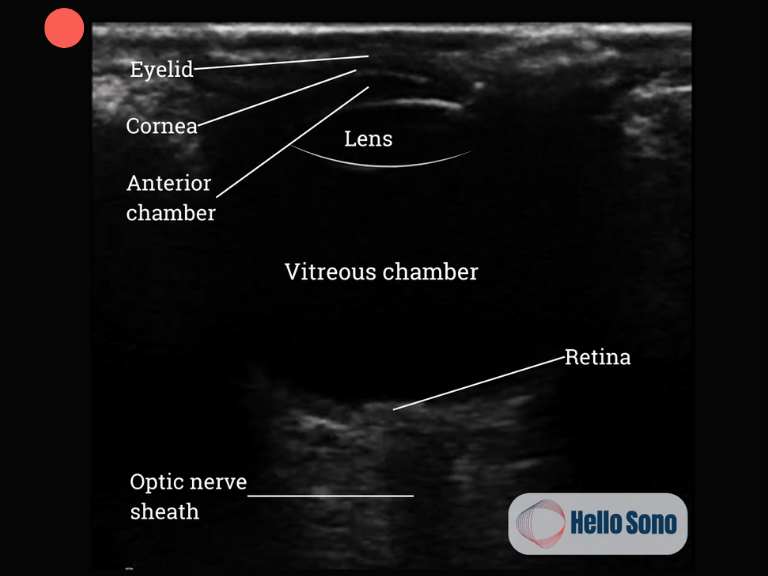
What a Normal POCUS Should Show:
In a normal ocular POCUS, the vitreous chamber should appear anechoic, with no mobile membranes or echogenic material. The retina is visualized as a smooth, continuous echogenic line at the posterior globe with no areas of detachment.
For additional examples of ocular pathology, such as posterior vitreous detachment and vitreous hemorrhage, see the downloadable Hello Sono Ocular POCUS Card.
Retinal vs Vitreous Detachment vs Vitreous Hemorrhage
When performing ocular POCUS, one of the most important skills is distinguishing retinal detachment from other posterior chamber pathology, as management urgency differs greatly.
Retinal detachment: Appears as a hyperechoic, undulating membrane that is tethered to the optic disc. It moves with ocular motion but remains anchored posteriorly and does not cross the midline of the globe. This is a vision-threatening emergency that requires same-day ophthalmology referral.
Posterior vitreous detachment (PVD): Appears as a thin, web-like echogenic membrane floating in the vitreous chamber. Unlike retinal detachment, it is not tethered to the optic disc and crosses the midline of the globe. PVD is common with aging. More than half of adults develop it by their 70s. While it can cause symptoms such as flashes and floaters, it is typically benign and not vision-threatening.
Vitreous hemorrhage: Appears as scattered, mobile echogenic particles that create a classic “snow globe” effect when the eye moves. It can result from trauma, proliferative diabetic retinopathy, or retinal tears. While not itself a retinal detachment, it often warrants ophthalmology referral, though not always emergently if vision is preserved.
The key differentiator for retinal detachment is the membrane’s attachment at the optic disc. Recognizing this finding helps providers distinguish it from the more common and usually benign posterior vitreous detachment or the swirling echoes of a vitreous hemorrhage.
Evidence:
The sensitivity of POCUS in diagnosing retinal detachment is consistently high across multiple prospective studies and meta-analyses. According to a multicenter prospective study published in JAMA Network Open, emergency department–performed ocular POCUS demonstrated a sensitivity of 96.9% (95% CI, 80.6%-99.6%) for retinal detachment. This finding is supported by systematic reviews and meta-analyses, which report pooled sensitivities in the range of 94% to 97% for POCUS in this setting.[1-2] The American College of Emergency Physicians, in its 2023 ultrasound guidelines, also cites meta-analytic data showing POCUS sensitivity of 94.2% for retinal detachment, reinforcing its utility as a rapid diagnostic adjunct in the emergency setting.[3]
Compared to dilated fundoscopic examination, POCUS can be performed quickly and effectively in outpatient and urgent care settings, especially when the funduscopic exam is limited. This translates to expedited ophthalmology referral and timely vision-preserving intervention.
Case Resolution:
The provider recognized the retinal detachment on ocular POCUS and urgently referred the patient to ophthalmology. The patient was seen the same day and underwent prompt retinal repair, preventing progression to central vision loss.
Impact of POCUS:
In this case, POCUS enabled rapid bedside diagnosis of a sight-threatening condition. Without ultrasound, referral may have been delayed. Ocular POCUS gave the provider immediate confidence to expedite care, ensuring the best chance of preserving vision.
Conclusion:
Retinal detachment is a vision-threatening emergency that can present subtly, particularly when central vision remains intact. Point-of-care ultrasound empowers primary and urgent care clinicians to make this diagnosis rapidly at the bedside. By shortening the time to ophthalmology referral, POCUS is instrumental in improving patient outcomes.
Ready to take the next step with POCUS?
Hello Sono helps practices roll out high-quality, compliant, and profitable POCUS programs.
Authored by Dr. Tatiana Havryliuk
References:
Gottlieb M, Holladay D, Peksa GD. Point-of-Care Ocular Ultrasound for the Diagnosis of Retinal Detachment: A Systematic Review and Meta-Analysis. Acad Emerg Med. 2019 Aug;26(8):931-939. doi: 10.1111/acem.13682. Epub 2019 Feb 5. PMID: 30636351.
Propst SL, Kirschner JM, Strachan CC, Roumpf SK, Menard LM, Sarmiento EJ, Hunter BR. Ocular Point-of-Care Ultrasonography to Diagnose Posterior Chamber Abnormalities: A Systematic Review and Meta-analysis. JAMA Netw Open. 2020 Feb 5;3(2):e1921460. doi: 10.1001/jamanetworkopen.2019.21460. PMID: 32074291.
Ultrasound Guidelines: Emergency, Point-of-Care, and Clinical Ultrasound Guidelines in Medicine. Ann Emerg Med. 2023 Sep;82(3):e115-e155. doi: 10.1016/j.annemergmed.2023.06.005. PMID: 37596025.