A Proven Strategy for POCUS Adoption: Compliance, Credentialing, and Quality Assurance
This article also appears in the POCUS Point-of-Care Ultrasound Certification Academy at this link.
Point-of-care ultrasound (POCUS) has emerged as one of the most transformative tools in modern medicine. It gives clinicians the power to make faster, more informed decisions—right at the bedside. But as more healthcare organizations and medical practices recognize its value, one big question often comes up:
How do we implement POCUS in a way that’s effective, sustainable, and aligned with the standards of safe, high-quality care?
After helping many organizations—large and small, well-resourced and resource-limited—build their POCUS programs, I’ve seen what works. The most successful programs don’t rely on enthusiasm alone. They’re grounded in a three-part strategy: compliance, credentialing, and quality assurance.
Start with Compliance
Too often, compliance is treated as an afterthought. But it should be the starting point. Without clear guidance on documentation, scope of practice, and infection control, even the most motivated team can run into problems.
I’ve worked with groups where POCUS was being used regularly, but with no documentation, no image archiving, and no billing. Clinicians were making decisions based on their scans but leaving no record behind. That lack of structure not only limits the clinical value of POCUS—it also creates legal and operational risk.
When compliance is addressed up front, with well-defined protocols and EHR-friendly workflows, everything else becomes easier. Here’s how to lay the groundwork:
Define the scope of what POCUS can be used for in your organization. Identify core and advanced applications, outline who can perform them, and clarify what training is required. To get started view high-yield POCUS applications for novice users in primary care.
Build a workflow that ensures exams are stored securely and documentation is consistent and accessible in the EHR.
Establish protocols for infection control, device maintenance, and external device usage. Learn how to classify the risk of infection and disinfection needed based on the contact of the probe with the skin in this article.
Create a quality assurance plan to track and improve performance over time.
Develop clinical guidelines to help novice users make appropriate decisions about when and how to use POCUS in common scenarios. You may download Hello Sono’s sample POCUS DVT pathway to get started.
Credentialing Isn’t Optional
One of the most common misconceptions I encounter is that a short course or workshop is enough to make someone proficient in POCUS. It’s not. Competency in ultrasound requires more than just exposure—it demands structured education, guided practice, and formal assessment.
Without a credentialing process, you risk inconsistent care and unclear expectations. But with one in place, providers are more confident, administrators are more supportive, and your program has the legitimacy it needs to grow.
To create a credentialing pathway:
Develop a written credentialing policy based on your specialty’s guidelines, use cases, and available resources. The ACEP POCUS Guidelines are a helpful starting point.
Incorporate a mix of learning modalities—online didactics, hands-on training, supervised scanning, and exam review are the gold standards. In remote and under-resourced settings, simulation and tele-guidance can effectively supplement training to achieve POCUS competency.
Clarify supervision expectations for learners. For example, should they perform DVT scans independently or only on patients already getting a comprehensive vascular study?
Include ongoing requirements for maintaining credentials, such as annual CME, a minimum number of scans, or periodic assessments.
Quality Assurance Is Key
Even skilled providers need feedback. Quality assurance (QA) helps ensure that scans are performed and interpreted correctly—and that your program is continuously improving.
QA isn’t just about catching mistakes; it’s about building a culture of learning. It also protects your organization from risk by providing evidence that your providers are using POCUS appropriately and competently.
Here’s what a strong QA process looks like:
Set a realistic review target. For credentialed providers, reviewing 5–10% of scans is typically sufficient. For trainees, 100% of exams should be reviewed until competency is achieved.
Evaluate both image quality and interpretation. These are separate skills, and both need to be assessed.
Designate qualified reviewers and give them protected time to do the work. If internal reviewers are not available, consider hiring qualified external reviewers to get the job done.
Run monthly or quarterly group POCUS QA sessions to create a shared learning experience and uphold quality standards.
Maintain clear documentation of QA reports in case of audits or external reviews.
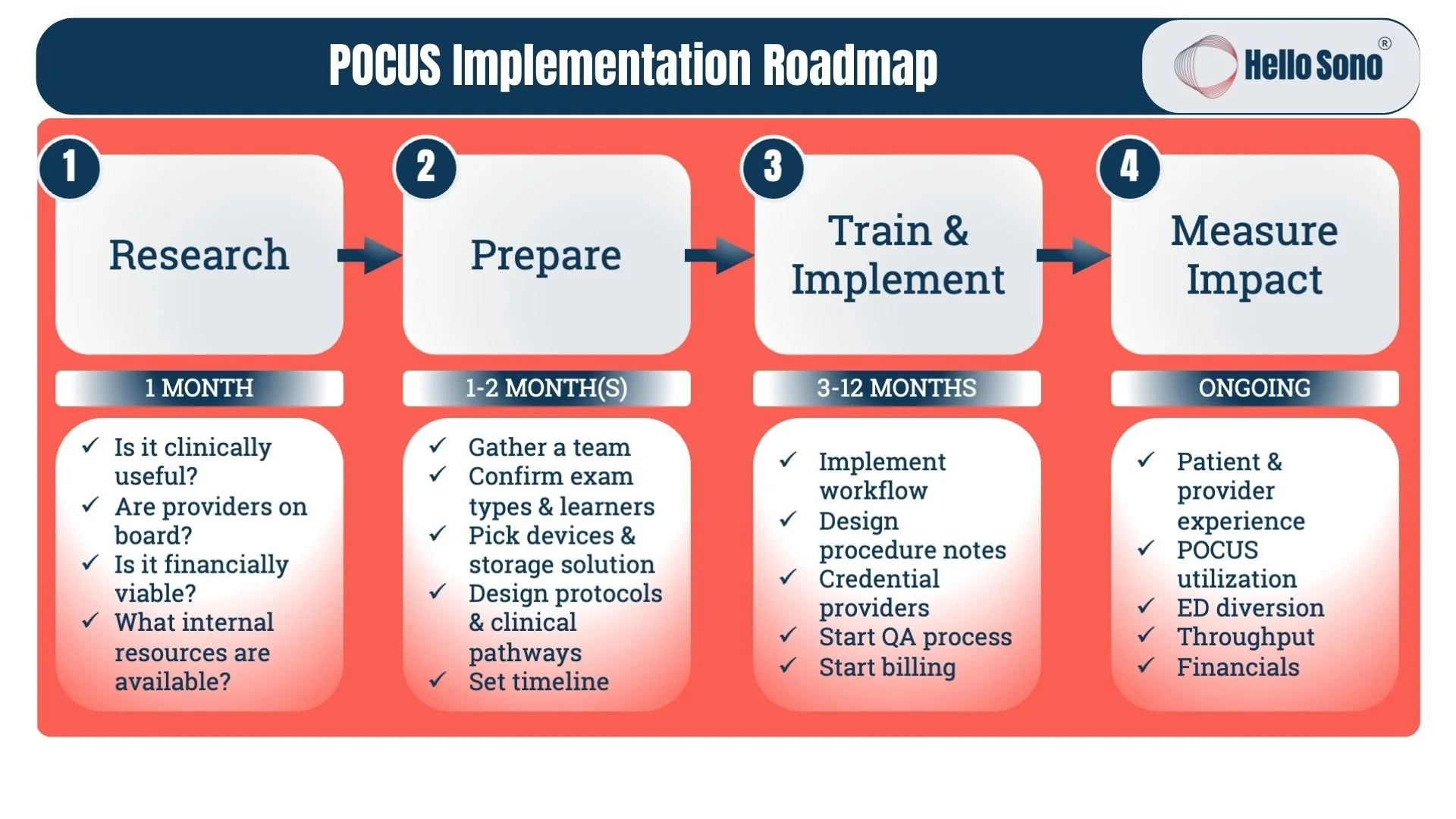
A Roadmap That Works
For anyone considering POCUS adoption, my advice is this: don’t rush it. Take the time to build a strong foundation. Get your policies in place. Support your providers with thoughtful training and credentialing. And make quality assurance an integral part of your culture from the beginning.
POCUS isn’t just a new tool—it’s a shift in how we think about diagnostics and decision-making. And when it’s implemented thoughtfully, it has the power to elevate care across every level of your organization.
About Dr. Havryliuk and Hello Sono:
Dr. Havryliuk is an emergency physician, formerly ultrasound director at the Brooklyn Hospital, and founder of Hello Sono. Throughout her 15 years of clinical practice, she has relied on POCUS to make informed clinical decisions whether it was in an urban ED, urgent care, or Everest Base Camp. Dr. Havryliuk is now on a mission to extend the benefits of POCUS to primary care and urgent care practices as well as rural hospitals by addressing the key barriers: lack of POCUS competency and infrastructure. Her team at Hello Sono offers in-person provider training and support with credentialing and implementation to build high-quality, compliant, and profitable POCUS programs. Hello Sono’s services include in-person workshops, exam review/quality assurance, and implementation support (workflow, curriculum, protocols, documentation, billing education).
Connect with Dr. Havryliuk on LinkedIn at https://www.linkedin.com/in/tatiana-havryliuk-md/.
Sign up for Hello Sono Newsletter and check out Hello Sono 2025 POCUS ROI Calculators at hellosono.com.